Molina Healthcare, Inc.
CEO : Mr. Joseph Michael Zubretsky
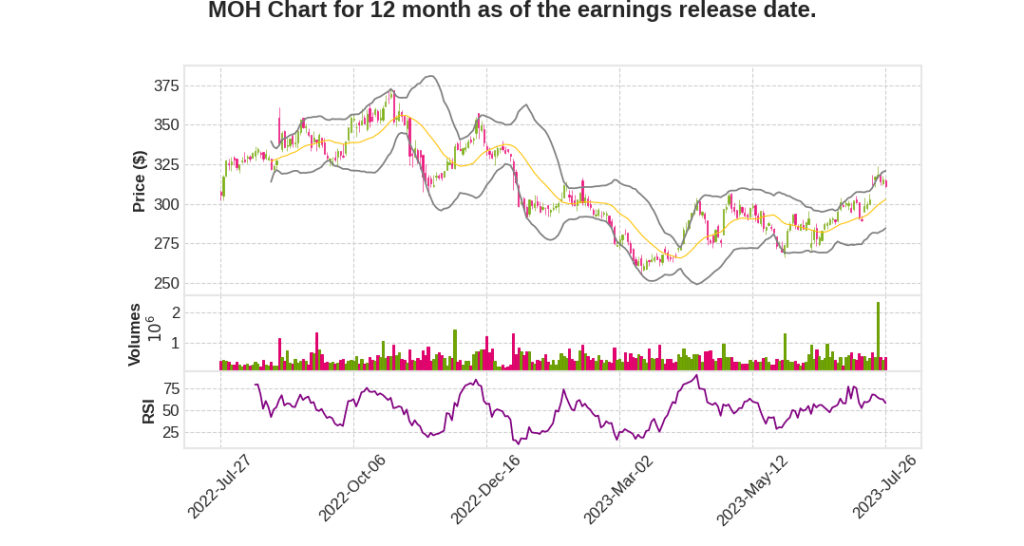
Quarterly earnings growth(YoY,%)
| Period | Revenue | Operating Income | EPS | Release Date |
|---|---|---|---|---|
| 2023 Q2 | 3.4% YoY | 22.7% | 23.5% | 2023-07-27 |
Mark Keim says,
Consolidated MCR and Medical Cost Management
- Consolidated MCR for Q2 2023 was 87.5%, reflecting strong medical cost management.
- Medicaid reported MCR was 88.3%, in line with expectations and target range.
- COVID-related costs have largely subsided.
Medicare Performance
- Medicare reported MCR was 89.2%, above long-term target range.
- Increased utilization of outpatient and professional services.
- Strong growth in D-SNP and MAPD products impacting new member margins.
Marketplace Performance
- Marketplace reported MCR was 73.7%, reflecting pricing strategy and seasonal patterns.
- Pricing strategy increased premium yield by approximately 9%.
- Well positioned to achieve mid-single-digit target margins for the year.
Balance Sheet and Financial Position
- Parent company cash balance was approximately $0.5 billion.
- Debt remained unchanged at 1.6 times trailing 12 month EBITDA.
- Low leverage position and ample cash and capital capacity for growth.
2023 Guidance
- Increased adjusted earnings guidance by $0.50 to at least $20.75 per share.
- Driven by Q2 operating and investment income performance and higher expected investment income in the second half of the year.
Redeterminations and Membership
- Medicaid membership down 93,000 from Q1 due to expected initial impact of redeterminations.
- Successful outreach protocols to help eligible members remain in the Medicaid program.
- Two-thirds of disenrollees potentially remain fully Medicaid eligible.
Joe Zubretsky says,
Second Quarter Highlights
- Adjusted earnings per diluted share for Q2 2023 was $5.65, a 24% year-over-year growth
- Premium revenue for Q2 was $8 billion
- Consolidated MCR for Q2 was 87.5%, at the low end of the long-term target range
- Adjusted pre-tax margin for Q2 was 5.3%, above the high end of the long-term target range
- Medicaid business had an MCR of 88.3% in Q2, in line with full-year guidance and long-term target range
- Medicare MCR for Q2 was 89.2%, above the high end of the long-term target range
- Marketplace MCR for Q2 was 73.7%, reflecting successful strategies to restore business to mid-single-digit target margins
2023 Guidance
- Adjusted earnings per share guidance for 2023 increased to at least $20.75, a 16% growth year-over-year
- Pre-tax margins are exceeding expectations
- Medicaid MCR is on target, Medicare slightly behind target, and Marketplace substantially better
Medicaid Redeterminations
- All but four states began disenrolling members in Q2
- Medicaid membership declined by 93,000 members in Q2, within expectations
- Impact on overall Medicaid MCR was negligible and within expectations
- States are willing to adjust rates to account for any changes in acuity or trend
Growth Strategy
- Premium revenue target for 2026 is $46 billion
- Recent state RFP wins drive over $5 billion in incremental premium revenue
- Acquisition of Bright HealthCare’s California Medicare Business, expected to add $1.8 billion of premium revenue
- Line of sight to approximately $38 billion of premium revenue in 2024 or 19% growth before additional strategic initiatives
- Long-term earnings per share growth rate target of 15% to 18% reaffirmed
Q & A sessions,
Impact of Risk Adjustment Liabilities
- Analysts projected a potential benefit of $66 million in positive development of risk adjustment liabilities.
- About half of this benefit is tied up in margins, reducing the overall impact.
- The retention of margins that don’t fall to the bottom line further reduces the potential benefit to less than half of the initial projection.
- The recognition of these risk adjustment liabilities is expected to occur largely in the first quarter with a little bit in the second quarter.
- This development is considered normal, similar to IBNR, and is anticipated to have a slightly favorable impact as it rolls off.
Power of Ex Parte and Reconnects
- Ex parte review, conducted in advance of any loss of membership, helps avoid eligibility loss.
- It is estimated that 40% of members lose their eligibility during the verification process, while 60% retain it.
- Of the 60% that retain eligibility, it is estimated that 50% do so through ex parte.
- CMS is encouraging states to increase ex parte efforts.
- Reconnects, which allow individuals to regain eligibility within 90 to 120 days, are crucial for members who lose their eligibility due to procedural reasons.
- Reconnects have the potential to retroactively cover claims and premiums back to the day of eligibility loss.
Outlook and Impact on Medicaid MLR
- The company’s outlook for redetermination process includes 800,000 members up, 400,000 members down, $1.6 billion in premium, and an 88.5% Medicaid MCR for the year.
- The company’s acuity determination and Medicaid MLR outlook remain unchanged.
- The Medicaid MLR outlook takes into account the slightly more favorable MCRs of levers compared to the portfolio average.
- Most states have minimum MLR or corridor programs, which the company operates efficiently and historically pays into.
- Any impact on medical margins from trends or yield would first be absorbed by significant liabilities already recorded for these conventions.
- The company reiterates confidence in the 88.5% Medicaid MCR estimate for the year.